Coronary heart disease: It can happen at any age

The latest data published by World Health Organisation (WHO) in 2020 stated that coronary heart disease deaths in Malaysia reached 36,729 or 21.86 per cent of total deaths.
The age-adjusted death rate is 136.21 per 100,000 of population, which ranks Malaysia #61 in the world.
As per the Department of Statistics Malaysia, ischemic heart diseases remained the principal cause of death with 17.0 percent of the 109,155 medically certified deaths in 2020.
Ischemic heart diseases remained as the principal causes of death for males at 19.3 per cent of the 65,918 medically certified deaths, and for females at 13.4 per cent of the 43,237 medically certified deaths in 2020. Of the 18,515 deaths related to Ischemic heart disease in 2020, 68.6% were males and 31.4% females.
National Heart Institute Consultant Cardiologist Dr Jayakhanthan Kolanthaivelu has revealed to Sinar Daily a few misconceptions that exist and what we should pay heed to with respect to coronary heart disease.
Dr Jaya shared that cardiologists have witnessed an increase in the number of young people suffering from heart disease across the country, partially attributed to the many changes in lifestyle over the years.
But before we get into that, let’s go back to basics and ask - what is heart disease?
Dr Jaya clarified that heart disease encompasses all the issues that a person could face owing to the improper functioning of the heart.
To simplify it further he said we should think of the heart like a pump, which requires oxygen supplied by the coronary arteries.
He explained how coronary heart diseases are caused by plaque or cholesterol buildup that could happen over the years with age or due to many lifestyle choices one makes.
He added that there are several circumstances that can accelerate the buildup of cholesterol.
“Diabetics or patients who have high cholesterol at a very young age, especially those with genetically or familial high cholesterol issues are more likely to be prone to the disease. Of course, there are also lifestyle issues like smoking and obesity which could contribute to a higher incidence of heart disease,” he said.
Who is most likely to be affected by coronary heart diseases?
Dr Jaya said that with the increase in stress and changes in lifestyle over time, more younger age group patients including millennials are being diagnosed with heart issues. According to him, the spectrum of the age group affected by the disease is fast changing to include those in their mid-30s and 40s.
But for people younger than that, do not sigh in relief and leave this page yet because the next few paragraphs may concern you.
Dr Jaya revealed his recent experience with a 23-year-old patient who had a heart attack and ended up being serious enough to have to be revived.
When tested, the patient’s coronary angiogram (a procedure that uses X-ray imaging to see your heart’s blood vessels) showed blood vessels which looked similar to that of a 60-year-old.
So, what had caused the healthy young patient to suffer heart attack?
In the case of this young chap, it was genetics. Dr Jaya revealed that this patient has a family health history as most of his family members suffered from coronary artery disease.
Another interesting fact he shared with us was that the youngest coronary heart patient he has seen was an 18-year-old.
“Earlier this used to be a rare scenario, only accounting for about two or three percent, but the incidence of heart disease in younger people is increasing. Coronary heart diseases may not be very common in the mid-20s but it does happen, and it is no longer a distant possibility for those in mid 30s and mid-40s,” he added.
Sadly, he pointed out that for some patients a heart attack could be the first and last symptom that they experience.
Dr Jaya further shared that there are many seemingly “healthy” people who come in for a routine medical check-up and end up shocked when diagnosed with heart disease.
So how does a cardiologist detect a patient with heart disease, a critical step to ensure the best treatment plan for the patient? Dr Jaya said there are a few tests used to determine if a patient has heart disease.
The first is a stress test. Patients are needed to run on a treadmill and ECG leads are attached to check for changes in the ECG.
There are multiple stages which measures these changes when both speed and elevation are altered on the treadmill. The changes in the ECG during the stress test may indicate possible coronary artery blockage.
Unfortunately, even if you pass the stress test with flying colours, it is still possible that you may be suffering from heart disease since the sensitivity of the test is only about 60-70 per cent.
However, this sensitivity can be improved by combining the stress test with other tests.
The CT scan is another test done by the cardiologist to evaluate the arteries.
The echocardiogram, another test Dr Jaya mentioned, is used to see your heart muscles and valves.
This test uses sound waves to produce images of your heart, allowing your doctor to see your heart beating and pumping blood. Your doctor can use the images from an echocardiogram to identify heart disease.
Dr Jaya highlighted that heart diseases have become more complicated with time, and he is seeing more patients suffering from complex blockages.
Since complex blockages are more challenging to treat, he stressed on the need to use technologically advanced methods to accurately detect these blockages and help plan the treatment.
But first, we need to understand what are complex blockages?
“When we talk about complex blockages, it basically involves either 100 percent occluded arteries, arteries blocked with calcium deposits (hardened cholesterol), or involving the left main,” said Dr Jaya.
The procedure used to treat blocked coronary arteries caused by coronary heart disease is called angioplasty, with most procedures involving either stents or balloons.
‘Stents’, Dr Jaya explained, work basically like ‘springs you put into the arteries’ to widen them.
So how does angioplasty work? Angioplasty is a procedure that opens narrow or blocked arteries to allow blood to pass through more easily to the heart muscles.
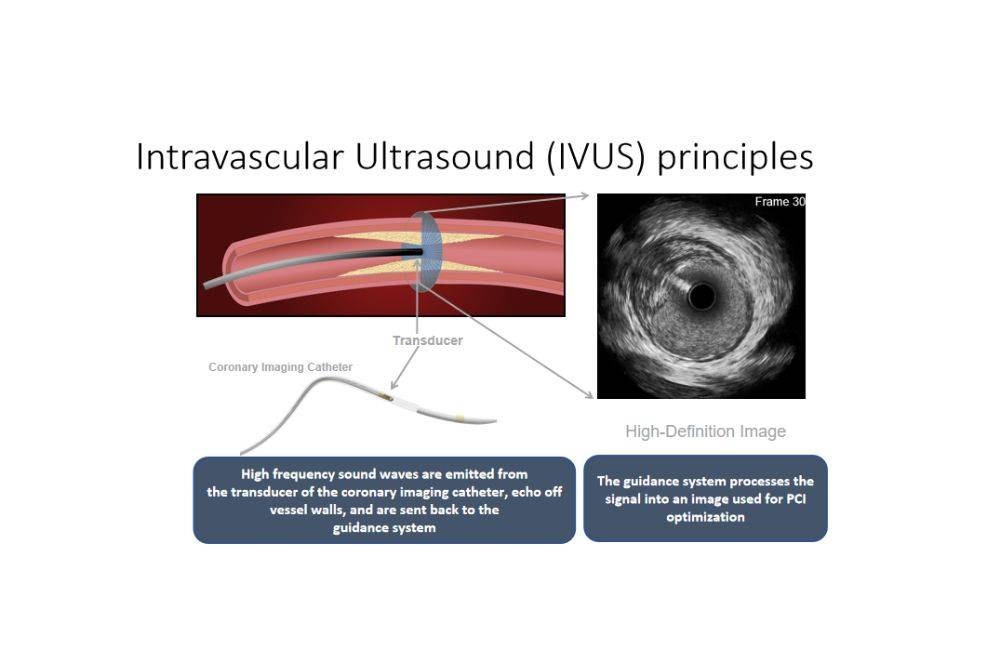
Dr Jaya explained that cardiologists use intravascular ultrasound as a tool to guide them in the angioplasty process.
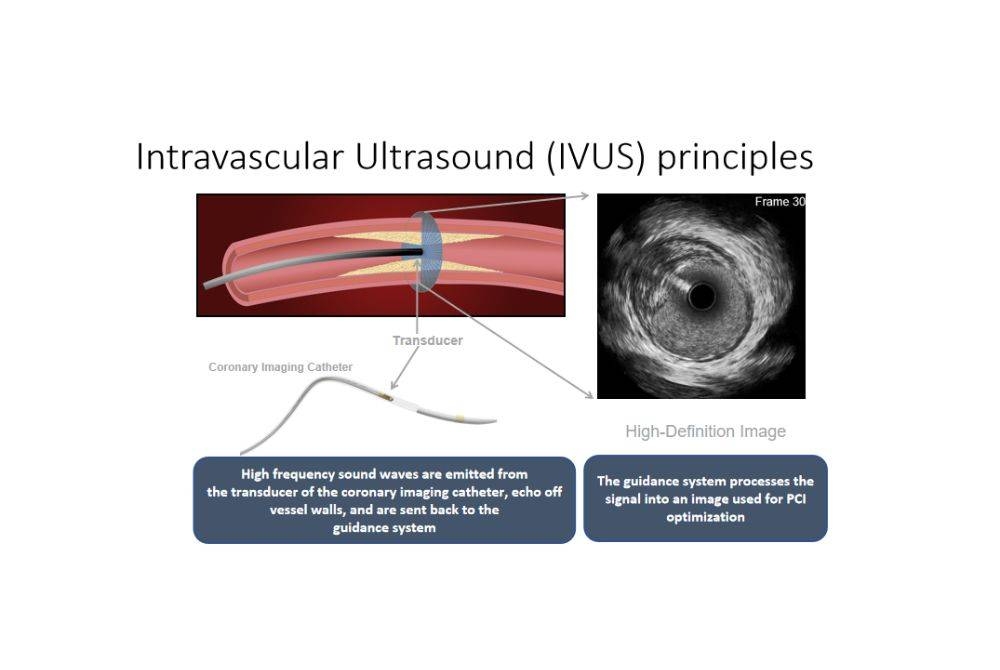
In layman terms, intravascular ultrasound is an imaging device used during the angioplasty procedure to better visualize the artery, determine the type of plaque formation, and provide information on the size of stents.
The information provided by the ultrasound is crucial for the cardiologist to check for the right size of stents to put into the artery, so that the stents can be optimized to the actual size of the artery to reduce risk of reocclusion.
Is angioplasty a painful and invasive process? Dr Jaya said the process involves minimal pain and is considered invasive since a wire is needed to be put into the coronary arteries.
“The access to the heart is either from the arteries in your hand or leg, where a tube will be placed. The tube goes all the way to your heart and the intravascular ultrasound will be passed along the tube,” he explained.
He added that the duration of the treatment depends on how complex are the blockages.
“We may not be able to use it for every patient, but an intravascular ultrasound would be the ideal way to accurately optimize stent placement if the patient doesn’t have financial constraints,” said Dr Jaya.
“Countries like Japan and Korea are able to cover the procedure through universal insurance, enabling the usage of intravascular ultrasound for everyone in the country undergoing coronary angioplasty,” he said.















