I don’t have diabetes. So why did I wear a glucose monitor for a month?
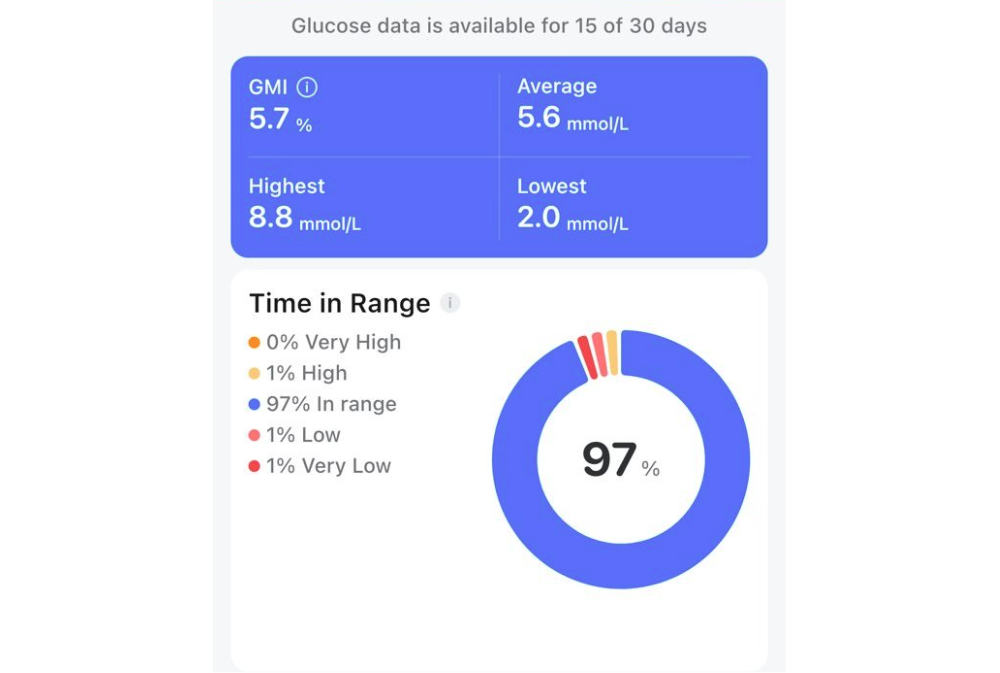
I started noticing patterns.

I don’t have diabetes. For 28 days I wore a continuous glucose monitor anyway. Not because I had to but because I was curious.
The device is usually prescribed for people managing diabetes, but it’s been making its way into the wellness space.
Influencers wear them, startup founders swear by them and TikTok is filled with charts of spiking blood sugar after oat milk lattes.
The idea is that more data equals more control. I wanted to see what it felt like to track my own body in real time.
The first monitor I tried was Abbott’s Freestyle Libre. It worked fine, but reading required a separate scanner. Carrying around an extra device and remembering to use it felt clunky.
Functional, yes, but inconvenient. Nevertheless, this certainly beats the traditional finger-pricking method.
Two weeks later I switched to another CGM that connected directly to my phone. Suddenly, the process was seamless. No gadgets to forget. Just open the app and there it was, my body translated into a tidy graph.
That was when I started noticing patterns. Rice and noodles may seem like interchangeable carbs, but my body treated them differently.
Rice pushed my glucose levels way up, while noodles with protein kept me steadier. Snacks I thought were harmless revealed surprising effects. And sugary drinks? My body reacted less to an iced cham than to a roti bakar with kaya and butter. I surely thought otherwise.
The graph reframed my decisions from guilty indulgences to tiny experiments. What will this do to the line?
The CGM also changed how I thought about movement. Whenever I saw a spike, I would take a quick walk.
Abbott’s nutrition team had told me even small bursts of activity could bring sugar levels down.
Watching the numbers dip or stabilise in made walking feel less like a chore and more like a button I could push to reset my system.
What struck me most was how visible small lifestyle choices became.
Eating slower, adding vegetables, getting up after meals – things I usually brushed off – showed up clearly on the graph.
The advice we always hear about balance and moderation wasn’t abstract anymore. It was right there, a line that rose or fell depending on what I did.
Wellness tech has been promising this kind of insight for years. Fitbits count steps, smartwatches track sleep and calorie apps log meals.
A glucose monitor is different because it doesn’t just tell you what you did. It shows how your body responded. That feedback loop, to me, is powerful. It made me care in a way step counts never did.
There are several types of CGMs and the right one depends on lifestyle.
For me, the app-based version was the only one I used consistently because it fit into my routine without effort.
But the monitor wasn’t just about numbers. It was about learning how to listen to my body in a new way.
The trend of people without diabetes using CGMs has its critics. Some say it risks turning eating into a neurotic numbers game.
But my month with the device didn’t make me obsessive. It made me curious. It didn’t push me to cut foods out.
It nudged me to rethink how I pair them and how I move afterward. For someone outside the medical system, that was enough.
Note: In Malaysia, continuous glucose monitoring devices are approved for use by people living with diabetes. The information provided is for general knowledge and educational purposes only, and it is not a substitute for professional medical advice, diagnosis, or treatment. You should always consult a qualified healthcare professional for specific medical concerns.
Download Sinar Daily application.Click Here!















